Abstract
Rare bleeding disorders (RBD) constitute 3- 5% of all inherited clotting factor deficiencies and include inherited deficiencies of fibrinogen (FI), factors II, V, VII, X, XI and XIII, and combined factor V and VIII, and affect both sexes in an autosomal recessive manner. Rare platelet disorders can also present with bleeding diathesis which are recessively inherited. Significant clinical heterogeneity is present in these disorders with varying bleeding symptomatology causing diagnostic and therapeutic challenges.
The objective of this study was to analyze the prevalence, characteristics, and treatment of rare bleeding disorders at the Valley Children's Hemophilia Treatment Center(HTC) in Central California.We conducted a retrospective analysis of all individuals who were referred for abnormal bleeding to our institution from 2018- 2023. We analyzed the clinical features, laboratory variables, and treatment of patients identified with RBD. Rare platelet disorders were included in this study. We excluded factor VIII, IX deficiencies and Von Willebrand disease (VWD) from this analysis.
Results
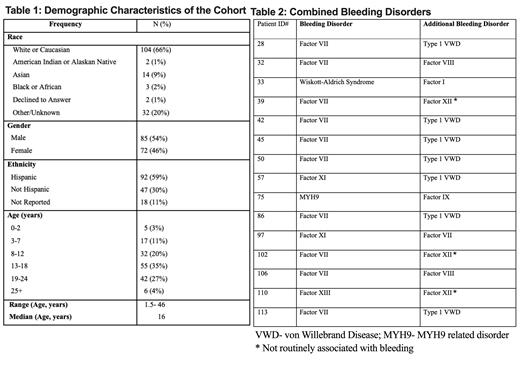
We identified a total of 157 patients (age range 18 months-46 years old) with RBD, 46% were of female gender (Table 1). Majority of the patients (n=92, 58%) were of Hispanic ethnicity. Major RBD in the cohort was Factor 7 (F7) deficiency (n= 96, 60.4%). F11 deficiency constituted 10.1%, followed by fibrinogen deficiency (6.3%), and F13 deficiency (5.7%). F2 and Plasminogen activator inhibitor-1 (PAI-1) deficiency was identified in one individual each. Glanzmann thrombasthenia was the most common platelet disorder noted in our population (n=7, 4.4%), followed by giant platelet disorder (n=6, 3.8%). MYH9- related disorder was identified in 5 (3.1%) individuals with macrothrombocytopenia and bleeding. Wiskott-Aldrich Syndrome was detected in 3 (1.9%) cases of RBD.
Combined bleeding disorders (CBDs) were observed in 15 individuals (9.5%) (Table 2). These disorders were distinguished by genotyping, factor activity, and chromogenic activity assays. F7 and Type 1 VWD combined disorder was observed in 46.7% (n=7) of these individuals.
Genetic testing was done in 38% (n=60) of the affected individuals. Genetic analysis was done through American Thrombosis & Hemostasis Network (ATHN 10) in 19% (n=30). F7 gene mutation was the most commonly identified mutation and variants c.1238G>A (p.Arg413Gln), c.1172G>A (p.Arg353Gln), and c.1091G>A (p.Arg364Gln) were observed in those with F7 deficiency. All individuals with F7 deficiency with variants of uncertain significance were presumed to be positive.
Treatment was specific to the factor deficiency. Most individuals received additional anti-fibrinolytic therapy during acute bleeding episodes. Recombinant F7 was used in platelet disorders for bleeding. Major bleeding events and death in the cohort was 1.2% (n= 2), and 2 individuals with F13 deficiency developed inhibitors to F13 concentrate. These individuals have been managed with recombinant F7 and anti-fibrinolytic therapy.
Conclusion
Ethnically diverse distribution of rare bleeding disorders was evident in our Central California cohort. Similar to previous reports, F7 deficiency was of the highest prevalence. A high prevalence of CBDs was also observed in this cohort. Genetic testing enabled diagnosis in some complex cases and needs to be used more widely to facilitate timely and accurate identification, and treatment of CBDs, and RBD in general. Further, these results help to identify novel mutations in different ethnicities, and provide additional information in understanding the clinical impact of new mutations.
Disclosures
Sathi:Vertex pharmaceuticals: Consultancy. Balasa:CSL Behring: Speakers Bureau; Sanofi: Speakers Bureau; Takeda: Speakers Bureau.